The following is a summarized review and update of currently available state and federal guidance as well as other published data that include recommendations from academic institutions and national medical societies. This informational statement should be used by clinicians in Virginia in keeping with their local/regional and organizational policies.
On March 25, 2020, Gov. Ralph Northam issued the Order of Public Health Emergency Two prohibiting elective procedures and surgeries in Virginia. That order expired at 11:59 PM on April 30, 2020. The Virginia Department of Health, in concert with the Governor’s Office, has issued guidance on resuming elective procedures in the Commonwealth. As of May 1, 2020, the Virginia Department of Health (VDH) recommends that all healthcare professionals refer to CMS guidelines, CDC guidelines and specialty society recommendations when considering resumption of non-urgent procedures and clinic visits.
General Recommendations
The Medical Society of Virginia (MSV) recommends adhering to core principles of safety for patients and healthcare personnel as licensed facilities begin scheduling elective procedures, including endoscopy. (1) The MSV encourages clinicians to refer to published guidelines, such as the American College of Surgeons’ ‘Roadmap for Resuming Elective Surgery after COVID-19 Pandemic,’ which includes guidance on timing for reopening of elective procedures; COVID-19 testing within a facility; PPE; case prioritization; pre-, peri-, intra-, and post-operative patient care; and data management. (2)
The MSV advises clinicians and licensed facilities to consider the following guidance before resuming non-urgent procedures, including endoscopy (1):
- Ensure that performing the procedure, in accordance with the commonly accepted standard of clinical practice, will not deplete facility or hospital capacity or the PPE needed to cope with the COVID–19 disaster
- Adequate staffing and supplies are available throughout the entire patient journey (presurgical, intra- and post-operative and during recovery in and out of the hospital), not detracting from local surge needs
- For hospitals, the ability to reserve at least 25% of its hospital capacity during Phase 1 of the Governor’s Forward Virginia Blueprint (beds, ventilators, staff, supplies, medications) for treatment of COVID-19 patients, accounting for the range of clinical severity of COVID–19 patients, and increasing that capacity to ensure all COVID-19 patients presenting to the facility are able to receive appropriate evaluation and/or care
- Ensure at least a 30-day supply of PPE both for universal precautions as per CDC guidance and any public source, whether federal, state, or local, for the duration of the COVID 19 disaster (3)
- Adherence to CDC guidelines to healthcare facilities for preparing and responding to community spread (e.g., all health system personnel and patients wear masks; limited visitation; promoting use of telehealth as an alternative to face-to-face visits where available or appropriate, etc.)
- Ensure a preoperative testing policy is developed and implemented
- Ensure sufficient testing capacity, including sample collection supplies and PPE, to perform diagnostic COVID–19 testing that adheres to the facility’s preoperative testing policy
- Ensure sufficient supply of pharmaceuticals related to the care of patients with COVID–19
The VDH recommends that clinicians and health care facilities consider the Medically Necessary Time Sensitive (MeNTS) method published by University of Chicago to prioritize non-urgent procedures, which includes 21 procedure-related, disease-related, and patient-related factors. (1, 4)
The VDH recommends that all healthcare professionals refer to CMS guidelines and specialty society recommendations for reopening clinical practices. In addition to exercising best clinical judgment, healthcare professionals should also consider current and projected COVID-19 cases in the facility and surrounding area; supplies of PPE; staffing availability; and urgency of procedures when making decisions about essential healthcare services. (1, 5)
Proper Use Of Personal Protective Equipment (PPE)
Per CDC guidelines, healthcare personnel must follow specific steps before caring for patients with confirmed or suspected COVID-19 (6):
- Receive comprehensive training on when and what PPE is necessary, how to don and doff PPE, limitations of PPE, and proper care, maintenance, and disposal of PPE.
- Demonstrate competency in performing appropriate infection control practices and procedures
Recommendations for Testing
Pre-procedural testing for COVID–19 is not mandated, and the decision to perform such testing should be based on local factors, including availability of tests, turnaround time for test results, and local prevalence of COVID-19 cases. Per MSV recommendations, “clinicians and healthcare facilities should consider making diagnostic COVID-19 testing available for patients undergoing sedation or anesthesia either through pre-op testing or through education to physician staff on specimen collection and guarantee of adequate PPE.” (1)
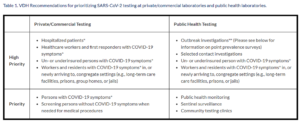
For practices planning pre-procedural SARS-CoV-2 testing, the following table was released by VDH on May 1, 2020 (7):
Local Prevalence of COVID-19 Cases
Although Governor Northam has authorized resumption of elective procedures and surgeries in Virginia, each health system, hospital, outpatient facility, and clinical practice must also consider local prevalence of COVID-19 to determine whether it is appropriate to begin expanding patient services (see Figure 1). The CDC, Johns Hopkins School of Public Health, New York Times, and Virginia Department of Health offer publicly available resources to determine the local spread of the infection.
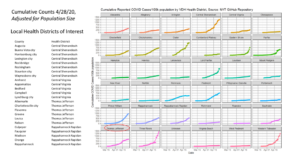
Figure 1. Cumulative incidence of COVID-19 by Virginia health district adjusted for population size (Source: University of Virginia, with data derived from New York Times reporting through 4/28/2020)
Referenced resources for clinicians are available below. In this dynamic environment, the Virginia Gastroenterological Society recommends that physicians and healthcare facilities continue to follow guidance from the Virginia Department of Health and the Governor’s Office to assure safe resumption of clinical services during the COVID-19 pandemic.
REFERENCES (accessed 5/1-5/2/2020)
- MSV FAQ: Resuming Non-urgent Procedures and Surgeries Available at https://www.msv.org/sites/default/files/faq_safely_resume_elective_procedures_v8_4.28_cc.pdf
- FACS Joint Statement: American College of Surgeons, American Society of Anesthesiologists, Association of periOperative Registered Nurses, American Hospital Association: Roadmap for Resuming Non-urgent Surgery After COVID-19 Pandemic Available at https://www.facs.org/covid-19/clinical-guidance/roadmap-elective-surgery
- Dept. of General Services – Division of Purchases & Supply (DPS): Emergency Vendor List Available at https://dgs.virginia.gov/procurement/resources/eva-emergency-vendor-list/
- University of Chicago: MeNTS Method for prioritizing non-urgent procedures Available at https://www.journalacs.org/article/S1072-7515(20)30317-3/pdf
- CDC: Get Your Clinic Ready for Coronavirus Disease 2019 (COVID-19) Available at https://www.cdc.gov/coronavirus/2019-ncov/downloads/Clinic.pdf
- CDC: Use Personal Protective Equipment (PPE) When Caring for Patients with Confirmed or Suspected COVID-19 Available at https://www.cdc.gov/coronavirus/2019-ncov/downloads/A_FS_HCP_COVID19_PPE_11x17.pdf
- Virginia Department of Health. VDH Updated Guidance on Testing for COVID-19. Available at https://www.vdh.virginia.gov/coronavirus/health-professionals/vdh-updated-guidance-on-testing-for-covid-19/